Blog
Managing Plantar Heel Pain

Plantar fasciitis is a painful condition caused by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel to the toes. This condition often results in sharp heel pain, especially with the first steps in the morning or after prolonged sitting. Common causes include overuse, wearing improper footwear, obesity, and tight calf muscles. To alleviate symptoms, a variety of treatment options are available. Custom orthotics can provide support and redistribute pressure, while night splints help keep the foot in a stretched position during sleep. Taping techniques and specific exercises can also strengthen the foot and improve flexibility. If you are struggling with heel pain or suspect you have plantar fasciitis, do not hesitate to seek professional help. It is suggested you schedule an appointment with a podiatrist who can assess your condition and tailor a treatment plan to get you back on your feet comfortably.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Jack A. Sasiene, DPM from Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Recognizing the Symptoms of a Broken Foot

A broken foot can be both painful and debilitating. Common symptoms include intense pain that worsens with movement, swelling, bruising, and difficulty bearing weight on the affected foot. You might also notice deformity or an unusual angle of the foot. In some cases, there may be a visible break through the skin, indicating a more severe fracture. Treatment for a broken foot typically involves immobilization, often with a cast or splint, to allow the bones to heal properly, and mild pain relievers can help manage discomfort. In more severe fractures, surgery may be required to realign the bones and stabilize the foot with screws or plates. If you suspect you have a broken foot or experience persistent foot pain, it is suggested you schedule an appointment with a podiatrist. This type of doctor can provide an accurate diagnosis and a comprehensive treatment plan to ensure a smooth recovery.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Jack A. Sasiene, DPM from Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Key Signs to Look for in a Broken Toe

Identifying a broken toe is important for timely treatment and recovery. One of the primary signs is a noticeable change in the toe's shape, as it may appear misaligned, crooked, or deformed. Severe pain is another common indicator, often sharp and intense at the moment of injury and persisting with movement. The affected toe might also show swelling and bruising, with discoloration appearing as a dark purple or blue hue. In some cases, there may be difficulty or discomfort when trying to move the toe. Prompt medical evaluation is essential for proper diagnosis and treatment, which may include rest, immobilization, or in severe cases, surgical intervention. If you have broken your toe, it is suggested that you consult a podiatrist who can offer you the correct treatment.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Jack A. Sasiene, DPM from Texas. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Are Bunions Affecting Your Everyday Life?
Dietary Guidelines for Gout

Gout is a form of arthritis caused by the buildup of uric acid crystals in the joints, leading to intense pain and inflammation, particularly in the feet. This condition often strikes the big toe, causing redness, swelling, and severe discomfort. To manage gout effectively, it is important to be mindful of dietary choices. Foods high in purines, such as red meat, organ meats, and certain seafood, should be avoided as they can increase uric acid levels. Alcohol and sugary beverages also contribute to the problem. Instead, focus on consuming low-purine foods like fruits, vegetables, whole grains, and low-fat dairy products. Staying hydrated by drinking plenty of water can help prevent uric acid buildup. Gout can cause intense foot pain, and completing daily activities may become difficult. If you have had one or more gout attacks, it is suggested that you are under the care of a podiatrist who can help you to manage this condition.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Jack A. Sasiene, DPM from Texas. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Effective Steps to Heal a Foot Wound

Healing a minor foot wound involves several important steps and visiting a podiatrist to ensure proper care and recovery. This doctor begins by gently cleaning the wound with mild soap and water to remove dirt and debris, then pats the area dry with a clean towel to avoid further irritation. He or she will guide you to use an antibiotic cream on the wound to prevent infection and promote healing. Next, the wound is covered with a sterile bandage or dressing, ensuring it fits snugly but comfortably to protect the area from dirt and bacteria. The podiatrist will explain how to change the bandage if it becomes wet or dirty, in addition to monitoring the wound for signs of infection such as increased redness, swelling, or pus. If you have a foot wound, it is strongly suggested that you are under the care of a podiatrist who can treat it effectively and safely.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Jack A. Sasiene, DPM from Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Pain in the Top of the Foot

Pain in the top of the foot can arise from various causes, often linked to issues with tendons, ligaments, or bones. Common conditions include extensor tendinitis, where the tendons that lift the toes become inflamed, or stress fractures from overuse or repetitive strain. Other potential causes include nerve compression, such as from wearing tight footwear or a condition like Morton's neuroma, and arthritis affecting the foot joints. Bruises or injuries can also lead to localized pain on top of the foot. Proper diagnosis is imperative for effective treatment, which may involve rest or changes in footwear. If you are experiencing persistent or severe foot pain, it is suggested that you consult a podiatrist for a proper diagnosis and treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Jack A. Sasiene, DPM from Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes of Painful Feet During Pregnancy

Pregnancy often brings about foot pain due to several factors. Collapsed arches, or fallen arches, are common as the body’s increased weight and hormonal changes put extra pressure on the feet, leading to discomfort and fatigue. Cracked heels can also develop as the skin becomes drier and less elastic, exacerbated by the extra weight and swelling. Swelling, or edema, is another frequent issue, where fluid retention causes feet to enlarge and feel tight, adding to the discomfort. These conditions can make walking challenging and painful. To manage foot discomfort during pregnancy, it is beneficial to wear supportive footwear, maintain good hydration, and practice gentle foot exercises. If you are experiencing foot pain during your pregnancy, it is suggested that you contact a podiatrist who can offer you effective relief techniques.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with Jack A. Sasiene, DPM from Texas. Our doctor will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton’s Neuroma Facts
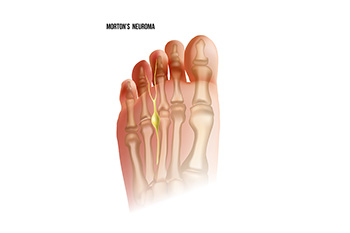
Morton’s neuroma is a painful condition affecting the foot, typically caused by a thickening of the tissue around one of the nerves leading to the toes. This condition often develops between the third and fourth toes, where the nerve becomes compressed or irritated. Morton’s neuroma can be triggered by factors such as wearing tight or high-heeled shoes, which place excessive pressure on the foot, or by repetitive stress from activities like running or jumping. Symptoms can include sharp, burning pain in the ball of the foot, tingling or numbness in the toes, and a feeling of having a pebble in the shoe. These symptoms often worsen with activity and improve with rest. If you have pain in this area of your foot, it is suggested that you contact a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Jack A. Sasiene, DPM of Texas. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Are You Suffering From Ingrown Toenails?
More...
Managng Achilles Tendon Injuries

An Achilles tendon injury can be painful and limiting, affecting your ability to walk, run, or engage in daily activities. This strong tendon connects the calf muscles to the heel and plays a vital role in movements like walking, jumping, and climbing stairs. Achilles tendinitis, often caused by overuse, results in stiffness and pain in the back of the heel, which can worsen with activity. If left untreated, this condition can progress to Achilles tendinosis, leading to further degeneration of the tendon. In severe cases, an Achilles tendon rupture may occur, causing sudden, sharp pain and making it difficult to walk. While treatment options vary based on the severity of the Achilles tendon injury, a podiatrist can provide both non-surgical and surgical solutions tailored to your needs. These may include targeted exercises, custom orthotics, or surgery to repair a ruptured tendon. If you have incurred an Achilles tendon injury, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Jack A. Sasiene, DPM of Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Essential Ballet Foot Exercises

Ballet foot exercises are vital for warming up, enhancing technique, and building foot strength. Begin with simple foot stretches to improve flexibility and prepare the muscles for intense activity. Point and flex exercises, where you extend and retract your toes, can help to increase your range of motion and strength. Performing demi-pointe and full-pointe exercises strengthens the foot muscles and improves balance. Additionally, toe rises and relevés, where you lift onto the balls of your feet, contribute to greater control and stability. Incorporating resistance bands into your routine can further enhance strength and flexibility. If you have developed a foot condition from not warming up properly before practicing ballet moves, it is suggested that you confer with a podiatrist who can treat any foot condition, and guide you on practicing correct foot stretches.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact Jack A. Sasiene, DPM from Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctor to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Is Hallux Rigidus?
 Hallux rigidus is a form of degenerative arthritis affecting the joint at the base of the big toe. This condition leads to stiffness, pain, and limited movement in the toe, often making walking or other activities difficult. The primary cause of hallux rigidus is wear and tear of the cartilage in the joint, which can result from repetitive use, injury, or genetic predisposition. People at risk for hallux rigidus include those with a family history of the condition, athletes, or individuals whose activities put repeated stress on the big toe joint, such as dancers or certain laborers. Treatment options vary depending on the severity and can include non-surgical approaches like targeted stretching exercises, anti-inflammatory medications, and custom orthotics to reduce pressure on the toe. In more severe cases, surgery may be necessary to alleviate pain and restore mobility. If you have big toe pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Hallux rigidus is a form of degenerative arthritis affecting the joint at the base of the big toe. This condition leads to stiffness, pain, and limited movement in the toe, often making walking or other activities difficult. The primary cause of hallux rigidus is wear and tear of the cartilage in the joint, which can result from repetitive use, injury, or genetic predisposition. People at risk for hallux rigidus include those with a family history of the condition, athletes, or individuals whose activities put repeated stress on the big toe joint, such as dancers or certain laborers. Treatment options vary depending on the severity and can include non-surgical approaches like targeted stretching exercises, anti-inflammatory medications, and custom orthotics to reduce pressure on the toe. In more severe cases, surgery may be necessary to alleviate pain and restore mobility. If you have big toe pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Toe pain can disrupt your daily activities. If you have any concerns, contact Jack A. Sasiene, DPM of Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Causes Foot Pain During Pregnancy?

Foot pain during pregnancy is common due to several factors. Weight gain places extra pressure on the feet, leading to arch collapse and overpronation. Hormonal changes cause ligaments to relax, affecting foot stability and contributing to conditions like plantar fasciitis or Achilles tendonitis. Swelling, or edema, increases discomfort, often affecting the feet and ankles due to fluid retention. To find relief, pregnant women can elevate their feet when possible to reduce swelling and wear supportive footwear with adequate arch support. Stretching exercises for the calves and plantar fascia can alleviate tension and strengthen muscles. Using compression socks or stockings can also help manage swelling. A podiatrist can diagnose causes of severe or persistent foot pain and ensure appropriate management throughout pregnancy. If you are experiencing foot pain during your pregnancy, it is suggested that you consult a podiatrist who can offer effective relief solutions.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Jack A. Sasiene, DPM from Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Lake Jackson, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.


